Hope For Children With Leukemia: Gene Therapy

The latest treatment for one of the most common cancers in children has not only managed to prevent the disease from spreading, but has also been able to reverse it. Gene therapy gives those suffering from leukemia in their B cells a new chance to live.
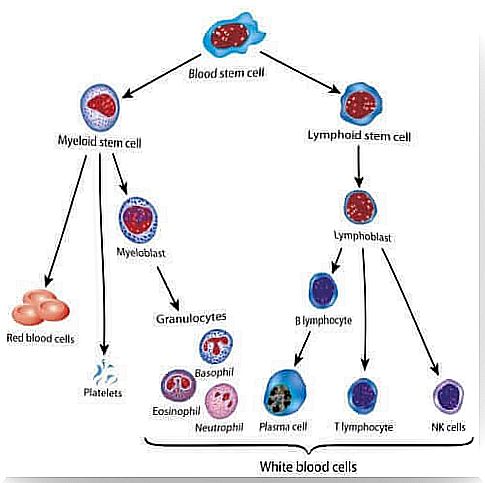
To understand leukemia, we must first understand the cells affected by the disease and how it develops. It all starts in the bone marrow, a spongy tissue that has a whitish color. It is located inside large bones such as the femur, hips and sternum.
The bone marrow contains a number of stem cells; these include lymphoid stem cells (lymphocytes), also called B cells, and myeloid stem cells (red blood cells, discs and some white blood cells).
So how does B-cell cancer start?
What is leukemia in children?
All forms of cancer begin when the body begins to produce cells at an uncontrolled rate. These abnormal cells are unique in that they do not die.
Given that the whole body is made up of cells, cancer can occur in any organ.
Types of leukemia in children
In accordance with their different characteristics, The American Cancer Society classifies childhood leukemia into several different subtypes. These are: acute or fast-growing, chronic, with myeloid cells or with lymphoid cells.
- Acute lymphocytic leukemia (ALL). This is the most common type of leukemia in children that involves the formation of white blood cells. It is also known as B-cell leukemia.
- Acute myeloid leukemia (AML). This type of cancer originates in myeloid cells. It represents the majority of other cases of leukemia.
- Chronic lymphocytic leukemia (CLL). This type of leukemia is rarely seen in children. It affects the white blood cells in the bone marrow.
- Chronic myeloid leukemia (CML). This variation originates in the fact that hematopoietic cells, which produce red blood cells and platelets, invade the bloodstream. It is uncommon in children.
There is now hope: Gene therapy
Recently, a clinic in Barcelona, Spain, treated several children with B-cell LLA who did not respond to conventional treatment. They used a new gene therapy – Tisagenlecleucel – which is still in its experimental phase in humans.
This treatment was approved by the FDA in 2012 and is distributed by the pharmaceutical company Novartis. But what exactly does gene therapy consist of?
Gene therapy
Gene therapy is a treatment that is adapted to each individual patient. It consists of introducing specific genes into the patient’s cells to fight the disease. In this way, they avoid possible rejection of the transplants and increase the effectiveness of the treatment by designing specific target cells that can attack the cancer.
To design a treatment for leukemia in children
The process consists of several steps and lasts for 22 days until it is complete.
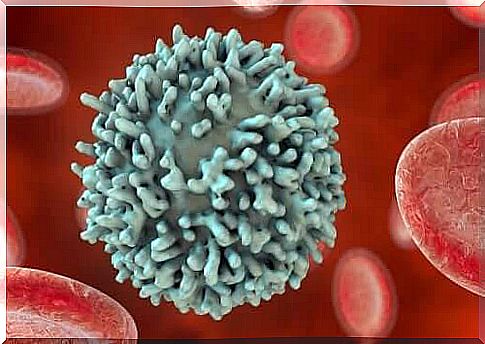
- First, specialists extract blood cells from the patient and isolate the T lymphocytes.
- They then genetically manipulate these cells in a laboratory. They insert a DNA sequence into them to produce a protein called a chimeric antigen receptor or CAR (Chimeric Antigen Receptor).
- The chimeric antigen receptor is responsible for recognizing another protein found on the surface of cancer cells, la CD19.
- The patient’s T lymphocytes (TL) that have undergone genetic modification continue to grow in the lab until there are billions of them.
- In the last phase, the modified T lymphocytes are given to the patient through an intravenous catheter.
How does the T-CAR / CD19 receptor pair work?
Imagine the cell as a sphere on whose surface stick-like structures protrude. Each of these structures has its own morphological properties. These sticks are responsible for the relationship between the cell and its environment and with other cells.
In leukemia, the person’s modified TL has a very concrete pin structure on its surface. CAR specifically recognizes a different stick structure on the surface of LB, CD10. Now that the T lymphocyte has recognized the cancerous B cell, it can start eliminating it.
According to Dr. However, Francis Collins, director of the National Institutes of Health, has many questions to consider before explaining the progress of cancer immunotherapy as an unconditional success.
Successes and failures of immunotherapy against childhood cancer
In the results, it was observed for three months after the treatment that 80% of the patients showed a clear regression of the disease. These were all patients who had a cancer that did not respond positively to conventional chemotherapy. The information comes from the National Cancer Institute .
But we must be careful with immunotherapy. Side effects have also been observed that experts cannot ignore. Dr. Collins presented a report on this issue in which he highlighted the following points:
- The CD19 protein is found in B lymphocytes, so LT-CDR does not differentiate between cancer cells and healthy cells. Thus, patients must undergo treatment for immunosuppression.
- The onset of cytokine release syndrome, which occurs during treatment.
- The occurrence of neurological side effects, such as confusion and seizures. These side effects seem to go away without the need for treatment.
Of course, this innovative treatment represents a new ray of hope for families whose children are suffering from cancer. Researchers are still optimizing the treatment, and it is still in an experimental stage.
But the results have been positive, to say the least, far above expectations compared to treatments for other cancers, such as HPV and malignant lymphomas.